Hallux rigidus is wear and tear of arthritis (osteoarthritis) of the great toe and is a chronic condition. It is not particularly related to osteoarthritis in other areas of the body and in most people it is not related to osteoarthritic conditions elsewhere in the foot and ankle. The key features are a stiffening of the movement through the main big toe joint, thickening /prominence particularly noticeable on the top of the foot and pain from the joint. The X-ray on the left shows an arthritic joint and on the right a healthy big toe join with a well preserved joint. Like osteoarthritis in other joints there are a spectrum of presentations.

Arthritic big toe with osteophyte
to a more continually painful joint. Eventually pain may be present throughout most weight bearing activities or even be present regardless of whether a patient is weight bearing on the foot or not. As with other arthritic conditions the progression of hallux rigidus is unpredictable and may not necessarily occur. Pain due to hallux rigidus of the big toe is very variable and may not correspond particularly well to any x-ray or clinical features such a limited joint movement.
Most commonly the cause is multifactorial. This means a combination of reasons, partly inherited partly related to previous activities/events. It can also occur as the end point of an inflammatory arthritis such as rheumatoid arthritis or gout. In most people, however, it is not related to these conditions. Very occasionally it occurs as a direct result of an injury to the joint .
Bunions & Hallux rigidus
It is certainly possible to have a bunion and hallux rigidus at the same time. Read the bunion section for an explanation of the bunion deformity and its treatment. Usually one condition is more of a problem than the other. The nature of the surgery is generally decided by which the more prevalent problem is and the surgeries are different. For example if there were only mild arthritic symptoms with a more painful bunion then a debridement of the joint (a small operation, see below) could be combined with a correction of the hallux valgus(bunion).
If the arthritic symptoms are more problematic then the main operation should be aimed at this with most commonly a Big Toe Fusion operation which allows both correction of the deformity and loss of the arthritic symptoms . These pictures below illustrate such a case with an arthritic bunion as well as lesser toe deformities. Here the left foot has undergone a fusion of the big toe and correction of the lesser toes.


A combination of the level of pain, radiographic stage of degeneration, the presence of deformity and the chance of success versus the degree of restriction following treatment helps the clinician & patient to reach an informed decision as to which of the many therapies will be most appropriate.
 |
 |
Intelligent choice of footwear
Armed with the knowledge that the foot and ankle simply acts mechanically as a system of rockers (the heel rocker rolling onto the mid-foot rocker which rolls onto the forefoot rocker), allows one to make a logical decision as to footwear that will help the condition.
To have entirely normal and comfortable gait pattern the foot does not have to “actively rocker” through these different areas. If the foot is supported in a shoe with a sole that curves through from heel to toe this prevents the foot bending at any of these points. This minimises the force through these joints and pain if the joints are arthritic (and can help with arthritis effecting the ankle or midfoot too)
A good starting point from arthritic big toe is to try using a fitflop type shoe. A wedge or platform shoe is also likely to work for women and for casual wear a stiff soled walking type boot would help most people.
Orthotics
Insoles support the arch profile of the foot and help transfer weight away from the forefoot area.
Injections
This is a small procedure which is normally carried out in the outpatient setting. Injecting the arthritic big toe joint just takes a few minutes to do. Symptoms will occasionally flare up temporarily after the injection for a few days or so and there is a very very small risk of infection after an injection. In “early” stages of big toe arthritis, and sometimes even in later big toe arthritis, it can provide good temporary relief. The best case scenario is that there may well be a 6 to 12 month improvement in the symptoms suffered. This will not affect the underlying natural history (likely progression) of the condition.
There are a number of possibilities and these may either preserve the joint or involve fusion or removal of the big toe joint.
A debridement (“tidy-up”) is used for earlier arthritis and can be performed with an open operation or minimally invasive technique. The joint can be realigned also and better sections of joint surface brought into play over worn out sections. These operations are known as osteotomies (such as a Moberg osteotomy). Sections of the joint surface can be replaced with implants that mimic cartilage or joint replacements that replace half or the whole joint. All replacements will in time wear out (though you may wear out first).
A fusion of the big toe joint is probably the most dependable , robust and long-lived option of all.
The first point to make is that it is difficult to define exactly who will benefit from a minimally invasive debridement of the big toe joint.
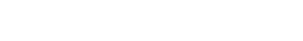
There is no hard and fast scoring system or objective assessment of the symptoms, x-rays and physical signs which allow unequivocal identification of patients who will benefit from the technique. In general, however, the type of patient who is likely to benefit from minimally invasive big toe debridement will still have a reasonable degree of joint space left on plain x-rays, pain towards the end of their range of movement (as opposed to throughout the range of movement from the big toe) and an absence of pain at night or at rest. An MRI is a sensible form of imaging to use when considering salvaging the Big toe joint. The scan below shows a joint that would be appropriate for a debridement with a prominent spur and well preserved joint .
The operation is carried out as a day case and usually under a general anaesthetic or a regional anaesthetic. Three small incisions are placed around the big toe joint..
The first part of the operation is to remove the prominence of bone on the top of the joint known as a spur ( or mote correctly Cheilus)

This is done with the minimally invasive technique by making a “pocket” in the sub-cutaneous tissue, down onto the bone and then using special minimally invasive burrs to carefully grind down the prominent bone. This part of the operation generally removes the prominent bone from the top of the foot and also increases the range of movement. The concavity seen at the joint in the right hand picture is the location of the metatarsal head spur seen in the above image. The ridge still evident is simply the base of the normal toe .


The final part of the operation is putting a small camera and shaving probe in to the joint to remove any debris from the first part of the procedure as well as any loose flaps of cartilage or inflammatory tissue. The incisions used for this are very small, of the order of just a few millimetres and this results in advantages. Generally the level the pain is far smaller than if the operation is done with open technique and in addition the amount of swelling to be expected is less. This combination of advantages also allows early mobilisation of the joint, usually from 1 week post surgery, which may give a greater chance of maintaining any increase in range of movement which occurs during the operation.

Pain relief
Some type of nerve block will be used during the operation to provide comprehensive pain relief for between 12 -24 hours after the operation.
Most people would need in addition a combination of painkillers for 2 to 4 days or so post operation. Most of the discomfort occurs in the first 24 to 36 hours and after this the level is generally not particularly severe.
Bandaging
The foot will be in a post operative bandage, just covering the front part of the foot. This provides excellent compression around the operative site and reduces the chance of bleeding and early post operative swelling. This compressive bandage can be removed at between 5 to 7 days post operatively but underneath will be adhesive dressings covering the operative scars and these need to be left intact for 2 weeks.
It is especially important the dressings are not disturbed unless they become wet. If they become wet they should be changed for dry dressings. The wounds themselves should not be interfered with for the first 2 weeks until the soft tissues have healed. If this is not adhered to then there is a risk that infection will be introduced in to the wounds and this will travel rapidly in to the underlying joint.
Post-Operative Mobility
It is possible to weight bear on the foot fully as soon as any nerve blocks have worn off. On the day of discharge patient normally has a post operative shoe which accommodates the bulky bandage. Once the bandage is removed it is possible to go in to a more normal shoe but generally one with a wider and supportive fit. A Fit Flop is good shoe at this stage post procedure.
This surgery is performed as a day case surgery.
After Discharge
Generally it will be helpful to use crutches for a day or two post surgery.
The post operative shoe will be helpful as long as bandages are worn and once bandages are removed a stiffer soled shoe is all that is required.
Driving can be undertaken in an automatic car from within a day or two if the left foot is operated upon. If a manual car is to be used then this is normally possible from a week or so post operatively.
Physiotherapy commences at a week post surgery to assist with a range of movement through the big toe as comfort allows. Exercises are encouraged on a daily basis for the first month or so post operatively.
Sutures are removed in the outpatient department at 2 weeks and it is not uncommon after this for the advice to be to keep the wounds dressed when in shoe wear to avoid the scars rubbing and the possibility of cellulitis developing.
How likely is it to work?
After the operation the bony prominence around the joint will be gone.
The chance of pain being significantly improved by the operation is in the region of 75 to 85%. This is broadly in-line with the results of debriding (tidying up) other arthritic joints such as knees, hips or ankles.
It is important to bear in mind two key points.
The first is that there is a 5% chance approximately that following the procedure the joint will become worse in terms of the severity of the pain. This, if it occurs, would likely necessitate fusion (or possibly replacement) of the joint. This is also a recognised feature with debriding arthritic joints elsewhere.
The second point to be born in mind is that with any arthritic joint being debrided the post operative course is usually reasonably protracted. It is likely to be 3 or possibly 4 months until it is evident just how successful the procedure has been.


A fusion procedure of the big toe involves getting new bone to form across a previously moving and articulating surface. The 2 bones (1st metatarsal and proximal phalanx) that have formed the joint are then permanently bonded together and movement no longer occurs at this articulation.
Given that this joint is the source of pain in big toe arthritis, once the joint is bonded and no longer moves the source of pain is gone and symptoms are lost.
The big toe has both a convex and a conave articulating surface. The joint surfaces are normally lined by cartilage which when healthy looks very like the type of surface one gets on a chicken drumstrick. If the joint becomes arthritic several things happen to the surface namely areas of loss of the cartilage lining, prominent spurs of bone form around the joint (called osteophytes) as well as inflammatory tissue occurs within the joint.

The fusion process involves removing all this unhealthy tissue and taking the articulating bone surfaces back beneath the normal cartilage and superficial bone to access the healthy bone that underlies the joint which has a good blood supply and readily form new bone once adequately exposed and stabilised.

Once the bone has been adequately prepared it needs to be positioned in an appropriate position in all planes. It needs to be positioned such that one can still roll forwards on the front part of the foot during normal walking, but not be elevated too much so that the tip of the toe does not make contact with the ground. The 2 images below show correct positioning with big toe sitting slightly off the ground at rest, the toe being able to contact the ground with the tip flexing .


This third image is shows the amount of heel rise that may be possible after a big toe fusion. How high the heel can get off the ground after the fusion operation is determined largely by the relative lengths of the two toe bones of the big toe and is also aided by a very flexible and hyper extendible inter-phalangeal joint (the one which is left mobile after fusion) which some patients inherently posses.

There is actually very little functional requirement for the big toe to move.
Ultimately after a big toe fusion, it can be expected that there will be very few restrictions upon activity.
Sport and function after Big Toe Fusion
You can drive a manual car from 5-6 weeks post surgery, when back in to more normal shoes. An automatic car can be driven sooner if the left foot has been operated upon.
In terms of returning to gym and sporting activity it is normally fine to use a static bike from 5 weeks post surgery, cross training from 7 weeks post surgery and lighter treadmill work from 9 weeks post surgery. Road running would normally need to wait for 12 weeks or so post surgery but may be possible to do this sooner if you are comfortable.
It would be normal to be able to return to running and sport wit a fused big toe.
In most cases it is likely that you will not fit in to the highest of heels following a fusion but this is not always the case (see Daily Mail article)

After the anaesthetic has worn off your foot should be largely free of pain, due to the use of the nerve blocks. You will be given a course of painkillers and anti-inflammatory tablets. These will be working for you when the nerve blocks wear off by 12 hours or so. You will need regular pain relief (in decreasing amounts) for the first few days after operation.
Bandaging/Dressings
Your foot will be in post operative bandage. This and the underlying dressings are left intact for the first week after which they are changed.
The foot will be more comfortable kept in an elevated position such as underneath a pillow when sitting down on a coach and on a single pillow when in bed at night. Position the foot slightly elevated, lessens the chance of it becoming swollen and feeling tight in the first 3 or 4 days post surgery.
Mobility
A physiotherapist will instruct you on the use of crutches and your post operative shoe. Generally you may put as much weight through the foot as you wish, within what is comfortable, as long as you remain in your shoe for walking. In some cases such as revision surgery or if your bone is soft your Surgeon may advise you just to put weight through your heel.
Outpatient Follow Up
You will be reviewed at 1 week post operation and have your dressings changed. You will need a few sutures to be removed at 2 weeks post surgery though the majority of the wounds closed with and absorbable stitch.
We generally advise that you keep the wound covered and dry during the third week post operatively but during the fourth week you may start showering it but still keep it covered with a dressing on a daily basis to avoid the wound running. The location of the wound at the inner aspect of the foot puts it at risk of rubbing when in the shoe wear. During the first 4 to 5 weeks post operatively, you will need to use the Donjoy post operative shoe.
At 5 weeks post surgery a check x-ray will be performed and if this shows good compression of the union and assuming the toe is pain free you will then be allowed to get back in to more normal shoes.
Driving is fine from 6 weeks and heavy manual activity from 10-12 weeks.
The choice of shoe wear is important initially and this should be something with a supportive and the stiff sole as well as something which can accommodate the swelling which will still be present post operatively. A good shoe to use at this stage post surgery is a Fit Flop type shoe for women an alternative would be a wedge or platform type shoe with appropriate fastening at the front to allow accommodation of the swelling during the course of the day.
Replacement of the big toe has a long history but the technique is still one very much in evolution. The “gold standard” would be being able to maintain movement whilst preserving good mechanical forefoot function with a joint replacement being predictably long lived. There are various options including 3 component replacements as shown , replacements of one side of the joint (hemi-arthroplasty) or sialastic hinge type joints where there is a flexible continuation of a spacer material across the joint space.

First MTP Fusion My symptoms were pain and swelling which made cross-country walking and tennis too painful to attempt. After I had my ankle fused at the first metatarsal joint and the many weeks of swelling around the operation site progressively reduced, I am totally free of pain and can once again enjoy walking and sports. The only long term penalty was the need to discard a few pairs of shoes and any post-operative discomfort was soon overcome.
R Dover Birmingham
First MTP Fusion I thank you for performing my surgery, I have been delighted with the results and am now back to playing 18 holes of golf with no difficulty whatsoever.
H Campbell West Midlands
Revision First MTP Fusion I would like to thank you for all the help and kind consideration that was shown to me last year when I was in need of an operation to repair my big toe joint. I visited the Foot and Ankle Clinic after previous surgery at another hospital, which did not prove to be successful. I can only say that the operation, which was performed went extremely well and I am now fully recovered. My stay at the Priory was only short lived, 2 nights, where I was treated extremely well by both the surgeon and the nursing staff. The advice I was given on how to look after my operation and my follow up visits have proven to be absolutely wonderful. Had it not been for the surgeon and the Priory Hospital I do not know what I would have done. I am now back at work following my accident at my former job. I can only say thanks for all the help and cooperation when I needed it most.
S Willetts West Midlands
1st MTP arthroscopy and minimally invasive cheilectomy
“I have had symptoms of pain in my foot for a period of 7 months. I was prompted to search for foot and ankle specialists. Happily I discovered Mr Mark Herron who was remarkably kind and informative and arranged an appointment. He listened to my version of symptoms and after a short discussion, he arranged an MRI scan within 5 days of the first meeting and a new appointment to discuss the MRI results within 3 days of the scan. It was suggested and I agreed to carry out an arthroscopy to remove a spur within 1 month. The operation on the 1st MTP joint required a minimally invasive cheilectomy and removing the offending spur. The operation time was short and I recovered and departed from hospital the same day, more comfortable, but in a little pain, than when I arrived.At the post-operative appointments Mr Herron was very gentle and explained in detail the surgery he had carried out and the remedial care to regain the pain and solution. I would recommend anyone to him for his professional expertise and care.”
Mr R Harding, 2017
Big toe (1st MTP) fusion
“It is 9 weeks down the line and I am delighted with progress. Importantly to me, I have started light running and up to 3 miles walking/running, mainly cross country along public footpaths. To keep me happy I aim to return to about 3 sessions weekly, total 20-25 miles a week and will build up to this gradually. The wound has almost healed with only a thin scar. The next goal is the Knowle Fun Run on 13 May (5 miles). I will let you know how I get on, as my running fitness should have returned by then. Kind regards and many thanks for the skilful job you have done.”
Mr G Lewis, 2012
Big toe (1st MTP) fusion
“Tomorrow is 12 weeks post 1st MTP fusion. … I unexpectedly ran the Leamington Spa Regency 10k run on Sunday. Successful and respectful time considering general lack of fitness. I think you have achieved a brilliant result for me – thank you again. Best Wishes, Mr G Lewis.”
Mr G Lewis, 2012
First MTP joint Fusion & Rheumatoid Forefoot Reconstruction From the initial consultation I was treated with courtesy and informed of every single aspect of the treatment to my foot. The operation was a complete success the staff very pleasant and as a result I am having my other foot done. The surgeon was very knowledgeable and skillful at his job. A Ashwin Warwickshire